| |||||||||||||
lunes, 2 de octubre de 2017
Obesidad / Obesity
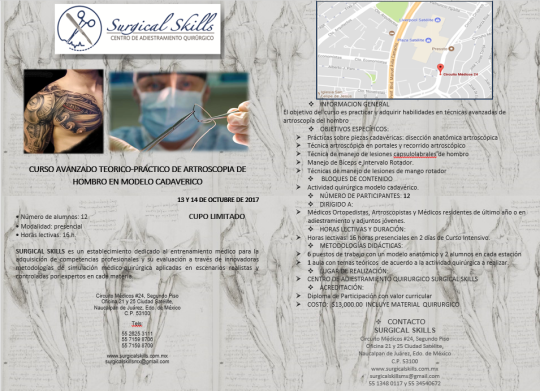
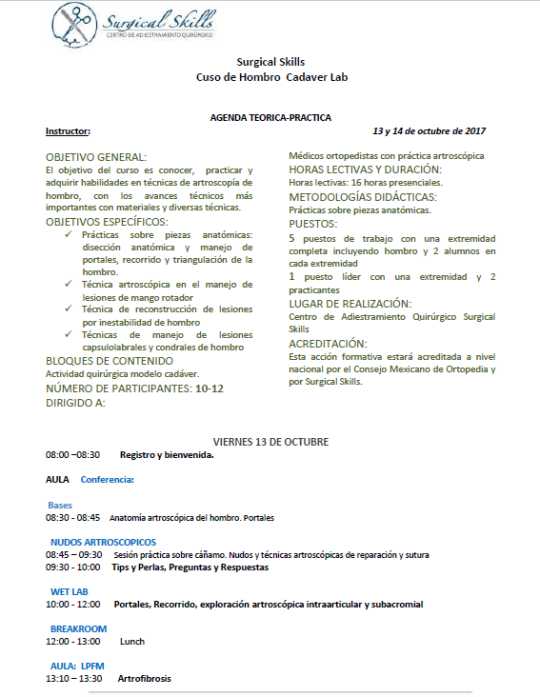
Surgical Skills Cuso de Hombro en espécimen biológico Lab
http://www.artroscopiayreemplazos.com.mx/academia/surgical-skills-cuso-de-hombro-cadaver-lab/
13 y 14 de octubre de 2017
Informes: 5526253111
13 y 14 de octubre de 2017
Informes: 5526253111
domingo, 1 de octubre de 2017
Origen y Tratamiento del Pie Equinovaro (Pie Zambo)
Entrevista al aire para el lunes 02 de octubre del 2017 a las 10:00 horas por TV Canal 21.2 ‘El Canal de la Asamblea Legislativa’ con la conducción de Pita Ojeda quien hablará sobre el tema de “Origen y Tratamiento del Pie Equinovaro (Pie Zambo)” con la participación del Dr. Juan Agustín Valcarce León, Médico Ortopedista Pediatra adscrito al Servicio de Pie y Tobillo en el Hospital de Ortopedia “Dr. Victorio de la Fuente Narváez”. La cita es en Av. Insurgentes Sur No. 1605, Col. San José Insurgentes, décimo piso de la Torre MURAL. (Junto al Teatro de los Insurgentes).

sábado, 30 de septiembre de 2017
Metabolómica y otros avances en la composición de la Leche Materna
Estimado Pediatra te invito al Seminario de Pediatría, Cirugía Pediátrica y Lactancia Materna. Continuamos el Programa 2017, el día 4 de Octubrebre las 21hrs (Centro, México DF, Guadalajara Liima Perú) a la Conferencia: “Metabolómica y otros avances en la composición de la Leche Materna”, por los “Dres. Daniel Fuentes Lugo y Horacio Reyes Vázquez“ Pediatras de la Cd del Carmen Campeche y CD de México”. La sesión inicia puntualmente a las 21 hrs.
Para entrar a la Sala de Conferencia:
1.- hacer click en la siguiente liga, o cópiala y escríbela en tu buscador
http://connectpro60196372.adobeconnect.com/metabolomica_lm/
2.- “Entra como Invitado” Escribes tu nombre y apellido en el espacio en blanco
3.- Hacer click en el espacio que dice “Entrar en la Sala”
5.- A disfrutar la conferencia 6.- Recomendamos que dejes tu Nombre Completo, Correo electrónico y que participes.
7.- Recientemente te solicita para emtar en la patafoem un add in, que es un parche bajalo de la siguiente liga: https://adobe.ly/2r4SSag
--
Dr. Enrique Mendoza López
Webmaster: CONAPEME
Coordinador Nacional: Seminario Ciberpeds-Conapeme
Av La Clinica 2520-310 col Sertoma
Monterrey N.L. CP 64718
Tel (81) 83482940, (81)81146053
Cel 0448183094806
jueves, 28 de septiembre de 2017
Resucitación prehospitalaria / Prehospital resuscitation
| |||||||||||
lunes, 25 de septiembre de 2017
Síndrome de embolia grasa y el cirujano de ortopedia y traumatología: lecciones aprendidas y recomendaciones clínicas
Fat emboli syndrome and the orthopaedic trauma surgeon: lessons learned and clinical recommendations
Fuente
Este artículo es originalmente publicado en:
De:
2017 May 30. doi: 10.1007/s00264-017-3507-1. [Epub ahead of print]
Todos los derechos reservados para:
Copyright information
© SICOT aisbl 2017
Abstract
PURPOSE:
Fat emboli syndrome is a rare but well-described complication of long-bone fractures classically characterised by a triad of respiratory failure, mental status changes and petechial rash. In this paper, we present the case of a patient who sustained bilateral femoral fractures and subsequently developed FES. Our aim was to review and summarise the current literature regarding the pathophysiology and management of fat emboli syndrome (FES) and propose an algorithm for treating patients with bilateral femoral fractures to reduce the risk of FES.
CONCLUSIONS:
Our algorithm for managing bilateral femoral fractures prioritises early stabilisation with external fixation, staged intramedullary nailing and conversion to plate fixation if FES develops. This protocol is meant to be the basis of future investigations of optimal treatment strategies.
KEYWORDS:
Bilateral femur fractures; Complication; Damage control orthopaedics; Fat emboli syndrome; Femur shaft fracture
Resumen
PROPÓSITO:
El síndrome de embolia grasa es una complicación rara pero bien descrita de fracturas de hueso largo caracterizadas clásicamente por una tríada de insuficiencia respiratoria, cambios en el estado mental y erupción petequial. En este artículo presentamos el caso de un paciente que sostuvo fracturas femorales bilaterales y posteriormente desarrolló FES. Nuestro objetivo fue revisar y resumir la literatura actual sobre fisiopatología y manejo del síndrome de embolia grasa (FES) y proponer un algoritmo para el tratamiento de pacientes con fracturas femorales bilaterales para reducir el riesgo de FES.
El síndrome de embolia grasa es una complicación rara pero bien descrita de fracturas de hueso largo caracterizadas clásicamente por una tríada de insuficiencia respiratoria, cambios en el estado mental y erupción petequial. En este artículo presentamos el caso de un paciente que sostuvo fracturas femorales bilaterales y posteriormente desarrolló FES. Nuestro objetivo fue revisar y resumir la literatura actual sobre fisiopatología y manejo del síndrome de embolia grasa (FES) y proponer un algoritmo para el tratamiento de pacientes con fracturas femorales bilaterales para reducir el riesgo de FES.
CONCLUSIONES:
Nuestro algoritmo para el manejo de fracturas femorales bilaterales prioriza la estabilización temprana con fijación externa, clavado intramedular escalonado y conversión a fijación de placa si FES se desarrolla. Este protocolo está destinado a ser la base de futuras investigaciones de estrategias de tratamiento óptimo.
PALABRAS CLAVE:
Fracturas bilaterales del fémur; Complicación; control de daños en ortopedia; Síndrome de embolia grasa; Fractura del fémur
Nuestro algoritmo para el manejo de fracturas femorales bilaterales prioriza la estabilización temprana con fijación externa, clavado intramedular escalonado y conversión a fijación de placa si FES se desarrolla. Este protocolo está destinado a ser la base de futuras investigaciones de estrategias de tratamiento óptimo.
PALABRAS CLAVE:
Fracturas bilaterales del fémur; Complicación; control de daños en ortopedia; Síndrome de embolia grasa; Fractura del fémur
PMID: 28555248 DOI:
Suscribirse a:
Entradas (Atom)




