| ||||||||||||
jueves, 8 de junio de 2017
Hipertermia maligna / Malignant hyperthermia
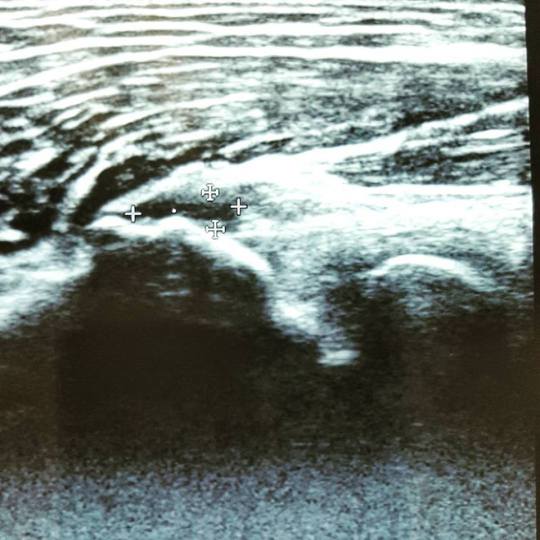
Ruptura parcial aguda del tendón extensor común del codo
Acute partial rupture of the common extensor tendon
Fuente
Este artículo es originalmente publicado en:
Este artículo es originalmente publicado en:
De:
2010 Jun;13(2):74-5. doi: 10.1016/j.jus.2010.07.002. Epub 2010 Aug 3.
Todos los derechos reservados para:
Author information ► Copyright and License information ▼
Copyright © 2010 Elsevier Masson Italy.
Abstract
Rupture of the common extensor tendon is the most common acute tendon injury of the elbow. The authors describe a case of a patient with a clinical history of tendinopathy caused by functional overload of the common extensor tendon, treated also with infiltrations of steroids, and subsequent partial rupture of the tendon during sport activity. The diagnosis was made clinically and at ultrasound (US) examination; US follow-up after some time showed the healing of the lesion. This case confirms that injections of steroids may be a contributory cause of tendon rupture, and emphasizes the sensitivity and specificity of US in the study of pathologies of the elbow tendons.
KEYWORDS:
Common extensor tendon; Elbow; Ultrasonography
Resumen
En inglés, italiano
La ruptura del tendón extensor común es la lesión del tendón agudo más común del codo. Los autores describen un caso de un paciente con antecedentes clínicos de tendinopatía por sobrecarga funcional del tendón extensor común, tratado también con infiltraciones de esteroides y posterior ruptura parcial del tendón durante la actividad deportiva. El diagnóstico se realizó clínicamente y con ecografía (US); El seguimiento de EE.UU. después de algún tiempo mostró la curación de la lesión. Este caso confirma que las inyecciones de esteroides pueden ser una causa contribuyente de la ruptura del tendón, y hace hincapié en la sensibilidad y especificidad de EE.UU. en el estudio de las patologías de los tendones del codo.
PALABRAS CLAVE:
Tendón extensor común; Codo; Ultrasonografía
PMID:23396798 PMCID:
DOI:
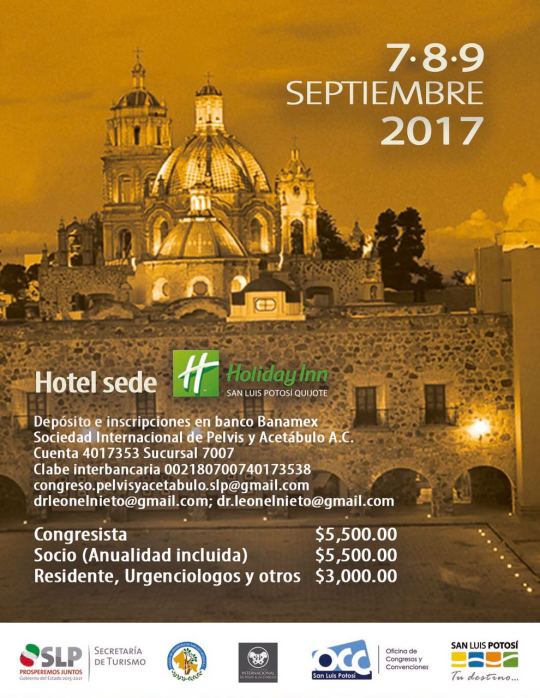
IV Congreso Internacional de la Sociedad de Cirugía de Acetábulo y Pelvis
a llevarse a cabo los días 7, 8 y 9 de septiembre en SLP, México.
Registro e inscripciones en:
Registro e inscripciones en:
miércoles, 7 de junio de 2017
OPTIMIZACIÓN DE ANALGÉSICOS PARA UNA MAYOR PARTICIPACIÓN EN LA TERAPIA DE EJERCICIO ENTRE PACIENTES CON OSTEOARTRITIS DE RODILLA Y DOLOR SEVERO: UN ESTUDIO DE FACTIBILIDAD.
Optimization of Analgesics for Greater Exercise Therapy Participation Among Patients With Knee Osteoarthritis and Severe Pain: A Feasibility Study.
Fuente
Este artículo es originalmente publicado en:
Este artículo es originalmente publicado en:
De:
2016 Mar;68(3):332-40. doi: 10.1002/acr.22682.
Todos los derechos reservados para:
© 2016, American College of Rheumatology.
Abstract
OBJECTIVE:
Severe pain in patients with knee osteoarthritis (OA) hampers the ability to exercise. A protocol for the standardized optimization of analgesics in combination with exercise therapy was developed. The purpose of this protocol was to reduce pain, thereby allowing the patient to participate in exercise therapy. The objective of the present study was to evaluate the feasibility and outcome of the protocol.
CONCLUSION:
The combined intervention of standardized analgesic prescription and exercise therapy allows most patients with knee OA and severe pain to participate in exercise therapy, leading to reduction of pain and activity limitations. These promising results need to be confirmed in a randomized controlled trial.
Resumen
OBJETIVO:
El dolor severo en pacientes con osteoartritis de rodilla (OA) dificulta la capacidad de hacer ejercicio. Se desarrolló un protocolo para la optimización estandarizada de los analgésicos en combinación con la terapia con ejercicios. El propósito de este protocolo fue reducir el dolor, permitiendo al paciente participar en la terapia de ejercicios. El objetivo del presente estudio fue evaluar la viabilidad y los resultados del protocolo.
CONCLUSIÓN:
La intervención combinada de prescripción analgésica estandarizada y terapia de ejercicios permite a la mayoría de los pacientes con OA de rodilla y dolor intenso participar en terapia de ejercicios, lo que lleva a la reducción del dolor y las limitaciones de actividad. Estos resultados prometedores deben confirmarse en un ensayo controlado aleatorio.
© 2016, American College of Rheumatology.
PMID: 26239403 DOI:
[Indexed for MEDLINE]
Free full text
Suscribirse a:
Entradas (Atom)


